How We Handle Recoupment Notices
Introduction
Recoupment notices can have a significant impact on a healthcare provider’s cash flow management. These notices, often issued months or even years after the date of service, require providers to return funds already reimbursed by payers. For many practices, this unexpected financial setback can disrupt daily operations, create administrative burdens, and result in unnecessary stress. At KMED billing, we specialize in helping healthcare providers navigate recoupment notices and protect their revenue.
The Challenge
One of our clients recently received a series of recoupment notices 1–2 years after services were rendered. The payer claimed that certain patients were not eligible for coverage during the dates of service. This unexpected demand for repayment caused:
-
Immediate disruption to the provider’s cash flow.
-
Hours of administrative time spent trying to review old claims.
-
Frustration over the lack of clarity and fairness in the payer’s communication.
Without expert support, this situation could have led to substantial financial losses.
Our Solution
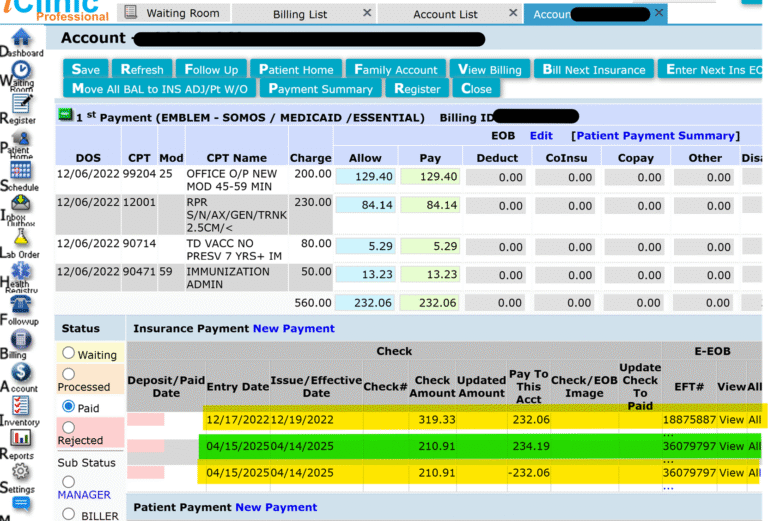
Our healthcare consulting team stepped in to handle the issue with a structured, evidence-based approach:
1: Investigating Recoupment Validity
We thoroughly reviewed the payer’s recoupment notices and compared them against original claim documentation.
2: Eligibility & Verification Checks
We conducted detailed eligibility and benefits verification for each patient in question to confirm whether coverage was valid at the time of service.
3: Patient Communication
Where lapses in coverage were identified, we proactively reached out to patients to clarify insurance changes and potential responsibility.
4: Drafting a Strong Appeal
We prepared a comprehensive claims appeal, supported by eligibility proof, patient correspondence, and legal references to payer policy.
Our appeal highlighted errors in the recoupment process and requested full reimbursement.
Our appeal highlighted errors in the recoupment process and requested full reimbursement.
Results
Our intervention led to a successful reversal of the recoupments. Not only was the provider repaid for the disputed claims, but the reimbursement amount was higher than the original payment, ensuring the practice recovered lost revenue while strengthening its financial stability.
This outcome demonstrates the power of a proactive, informed strategy in handling recoupment notices and claims appeals.
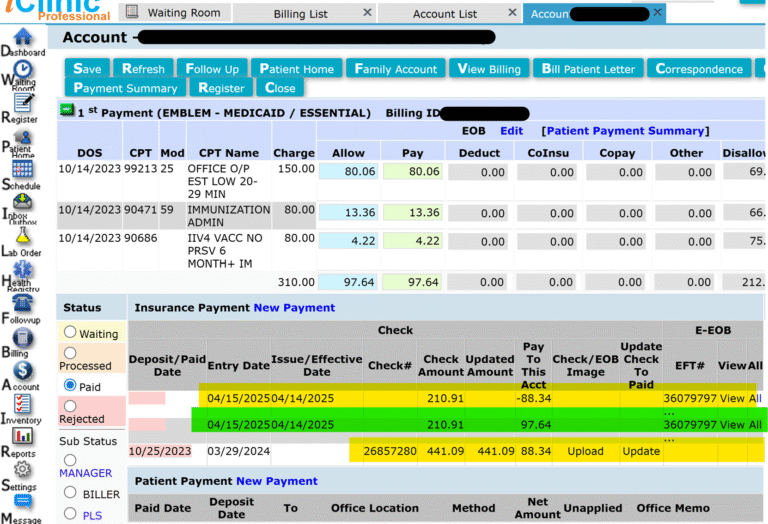
Here is another example below.